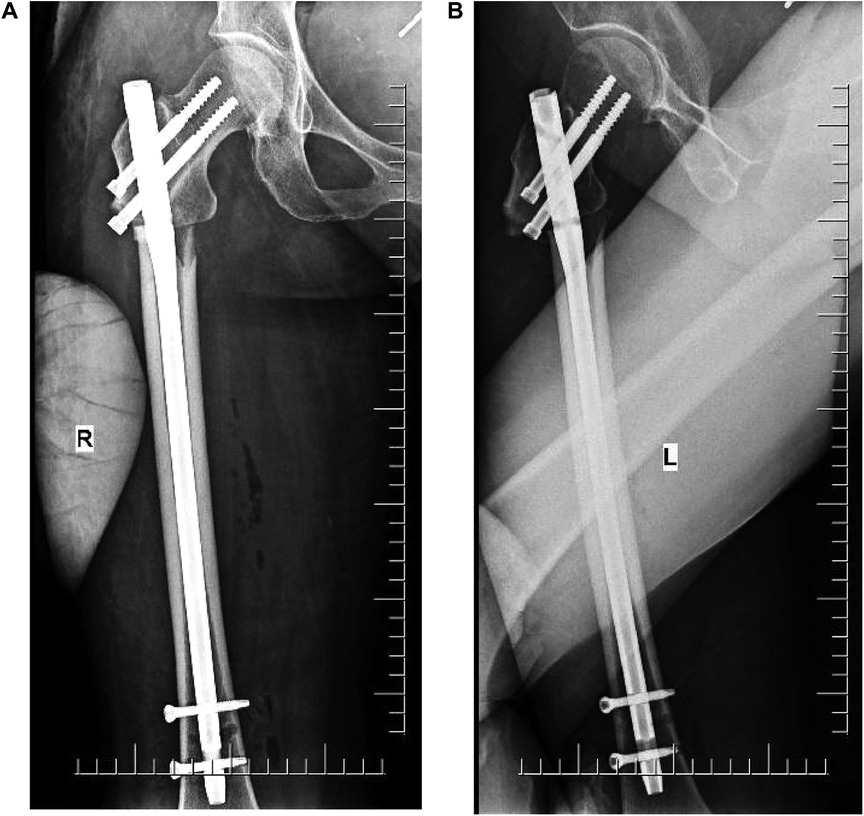
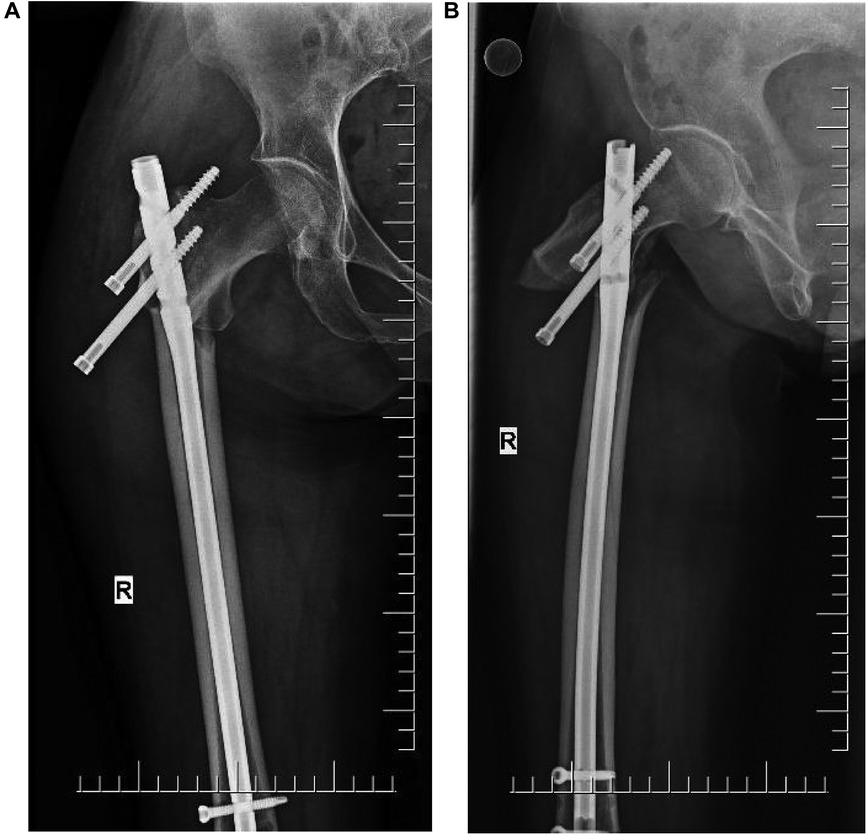
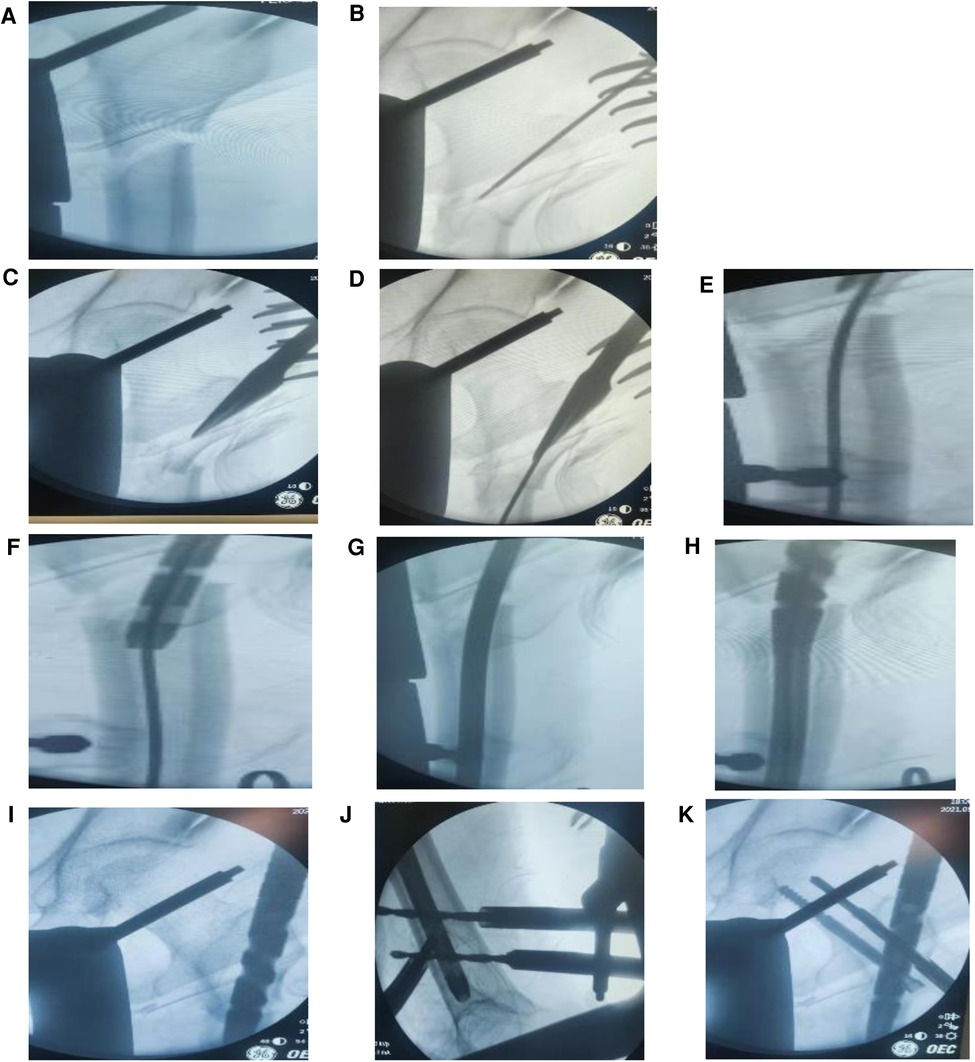
Reconstruction intramedullary nailing for a failed subtrochanteric Seinsheimer type IIB fracture: a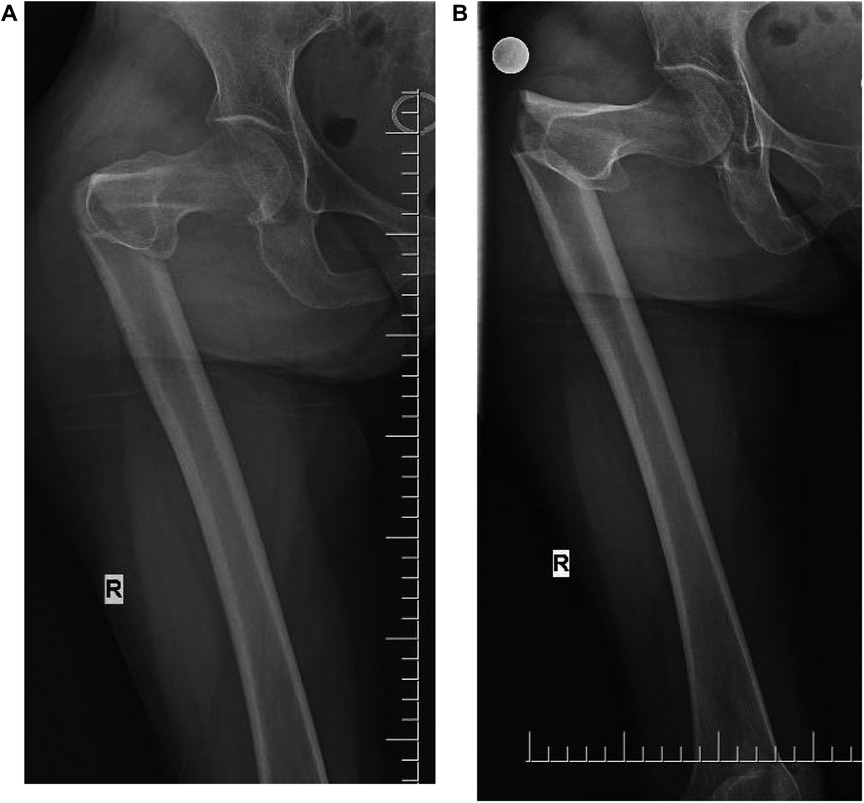 Introduction: Methods: Result: Conclusion: It is generally believed that a subtrochanteric fracture of the femur refers to the fractures between the upper edge of the small rough dragon and the site of femoral stenosis (1). Sometimes, the proximal end of the fracture continues to the large rotor, and the distal small rotor extends down the 5-cm range of the fractures (4, 2.1. Patient The patient was a seventy-year-old female with a subtrochanteric helical fracture of the femur due to a sprain from an accidental fall downstairs (torsion violence), who had a history of rheumatoid arthritis for over 10 years, which was controlled by self-medication. The patient's BMI (Chinese standard) was 45/(1.65) 2≈16.53 < 18.4, thin. No other basic diseases and family genetic history were recorded. 2.2. Diagnosis Anteroposterior and lateral radiographs of the femur showed a subtrochanteric spiral fracture of the femur with proximal posterior rotation, separation, and displacement of the broken ends and angulation (Figures 1A,B). The patient presented with tenderness and percussion pain along the longitudinal axis of the right lower extremity, as well as flexion shortening and valgus deformity of the right lower extremity. The right hip was obviously painful and swollen, and the functional activities of the right lower extremity were limited. The fractured part was similar in morphology to a “pseudo-joint.” The patient was positive for percussion pain on the longitudinal axis of the right lower limb. Subtrochanteric Seinsheimer type IIC fracture refers to a distal fracture of the small rotor. The two can be distinguished by x-ray and CT (Computed Tomography). Figure 1 FIGURE 1. (A) Anterior radiograph fracture with angular deformity. (B) The fracture was significantly displaced, with proximal posterior rotation. 2.3. Surgical process The patient was admitted to the hospital, and relevant examinations were conducted to exclude any contraindications of surgery. After reading the radiographic images, the surgeon decided to perform a minimally invasive incision treatment using a femoral reconstruction intramedullary nail with the consent of the patient and their family. After successful combined spinal-epidural anesthesia, the patient was placed in the supine position, bed traction of the affected limb was performed, the healthy limb was placed in the lithotomy position, the perineal blocking pad was placed in the groin of the unaffected side—with buttocks of the affected side being placed are as far away as possible—the bed traction was externally rotated under C-arm fluoroscopy, and abduction, manual squeezing, lifting, and pressing were also performed to reset the broken end (three points and one line: the midpoint of the groin–knee–ankle point was positioned on a straight line, and the toes were vertically upturned). After fluoroscopic observation of the alignment, the surgical area was routinely disinfected and covered with sterile towels and a brain surgical skin film. The anatomical projection of the apex of the greater trochanter was determined by hand touch, and an incision of approximately 5 cm was made obliquely from the proximal end to the distal end to the apex of the greater trochanter. Separation forceps were used to separate the surrounding tissues, the fascia was opened longitudinally, and the apex of the greater trochanter was touched. After the needle point was determined by fluoroscopy under the C-arm machine, with the aid of the sleeve, an opener was inserted obliquely at a 45° angle in the direction of the needle to the position of the minor trochanter. After completion, the long guide needle was inserted into the distal end, and the implantation and broken end of the guide needle was observed under the C-arm machine. An electric drill was used to expand the proximal medullary cavity, and then a 6.5-mm drill bit was used to expand the distal medullary cavity. According to the condition of the patient's medullary cavity, the distal medullary cavity was increased by 1 mm. Under the C-arm machine, the intramedullary needle implantation and broken ends were seen by fluoroscopy, and two locking nails were implanted along the distal end of the guide. The intramedullary needle was knocked back to shorten the separation between the broken ends, and the proximal double half-threaded screw was driven along the guide according to the perspective of the C-arm machine, which was satisfactory. After satisfactory surgery, rinse, suture, and bandage the wound. Remove the anesthesia tube and return to the ward. After the operation, antibiotic treatment was given for 48 h, and intervention treatment for anti-osteoporosis and promoting fracture healing was performed. The patient could stay in bed for 14 days and perform simple standing activities with the aid of an auxiliary device. One month after surgery, simple walking activities could be performed with the aid of an auxiliary device. After three months of surgery, the patient could gradually disengage from the auxiliary tool for autonomous activities. During this period, the patient avoided sitting for a long time to prevent nail peeling during nail cutting. The patient was instructed to undergo a routine X-ray examination at two month after surgery to assess fracture healing, hip joint morphology, and implant status. The patient and their family members did not undergo routine medical examinations as instructed. After two months of surgery, the patient consciously contacted the foreign body in the hip to receive reexamination. Radiographs were conducted four days after surgery (Figures 2A,B). The affected hip could be flexed and extended two months after the surgery. Self-reported hip pain was obvious, which worsened after activity, and screws and bone-like objects were palpable on the outer side of the proximal thigh. The radiographic images showed that the proximal double half-threaded screw and the proximal end of the intramedullary needle were prolapsed, and the broken ends were separated and displaced again. There was no obvious callus formation around the fracture zone (Figures 3A,B). Figure 2 FIGURE 2. (A,B) X-ray (4 days after surgery). The lateral end of the fragment shows a displacement. Figure 3 FIGURE 3. (A,B) X-ray (2 months after surgery). The proximal end of the nail was dislodged, and the broken end was displaced again. The incidence of Subtrochanteric fracture of the femur is approximately 25% among the elderly (12). Such fractures are mostly affected by factors such as osteoporosis and their own anatomical structure characteristics, biomechanics, and blood supply. Femoral fractures are caused by a slight external force (2, 5. Causes of failure and possible problems 5.1. Spiral fracture and instability Intraoperative reduction and separation, the limitation of traction maintenance, intraoperative reaming, and handle needle insertion are prone to fracture reduction deviation and implant failure. Older persons, poor constitution, and osteoporosis lead to insufficient nail stability and holding force, and cortical integrity damage leads to poor stability. The subtrochanteric area is the stress concentration area. From the perspective of biomechanics and anatomical structure, many scholars believe that the anatomical reduction of a subtrochanteric fracture of the femur, the integrity of the medial and lateral cortex, and the stability of the broken ends are very important for the success of surgery and the promotion of fracture healing (2, 5.2. No anatomical reduction Anatomical reduction of fractures is a key factor in the success of surgery (2, Figure 4 FIGURE 4. (A–K) The whole process of surgical traction reduction, needle threading, and nailing. Figure 5 FIGURE 5. After repair, PFNA and steel wire were used for internal fixation. 5.3. The entry point and opening position of the nail are on the outside, the medullary cortex ruptures, and the intramedullary needle slides (Figure 4B-D) It is mostly recommended that the needle insertion point should be located at the apex of the greater trochanter and the fossa ovalis (14). After the needle insertion point deviates slightly outside the apex of the greater trochanter, the intramedullary needle sticks to the proximal medial wall during the needle insertion process. Therefore, the needle insertion process becomes difficult, and the fracture is displaced, or the proximal cortex is penetrated during the forced needle insertion process. The weak part is freed from the outside of the medullary cavity, the intramedullary needle is drawn into the distal medullary cavity, or the posterior cortex is destroyed after the proximal reaming, which causes the intramedullary needle to stick to the posterior cortex, squeeze the proximal anterior side, and move into the distal medullary cavity. In addition, when the electric drill bit at the needle entry point was used to expand the proximal medullary cavity for the first time, the positioning point was displaced posteriorly due to the instability of the positioning needle or the rupture of the outer and posterior cortex. The intramedullary fixation failed due to the crushing damage to the bone cortex and the incomplete cortex itself during the entry of the electric drill. The patient was old, had been taking rheumatoid arthritis drugs over a long period, had a poor nutritional status, and had obvious osteoporosis. There was a risk that the intramedullary needle could deviate from the normal medullary cavity and break the cortex during the needle insertion process. Reaming of the medullary cavity leads to weak cortical strengthening or rupture and increases the risk of dislodgement or penetration of the nail out of the medullary cavity. The intramedullary needle is implanted according to the reduction situation and the fracture vertical line adjustment handle to ensure a satisfactory anatomical angle (Figures 4B–D). 5.4. The absence of lateral radiographs cannot determine whether the intramedullary pin is in the medullary cavity and the reduction of the fracture Intraoperative minimally invasive intramedullary fixation or intramedullary needle implantation has a blind spot. In addition, the fracture is unstable, or the cortical bone is damaged, and the distal and proximal fracture ends are likely to be separated again during the slippage of the implantation point and the needle threading process. The proximal intramedullary needle slides from the posterior wall into the distal intramedullary needle and is implanted into the medullary cavity, resulting in a false impression of good implantation, and x-ray fluoroscopy shows a false good reduction and implantation (Figures 4E–I). Therefore, a perfect frontal and lateral radiograph is particularly important at this time to locate the intramedullary needle and assess the fracture (14). 5.5. The operator's proficiency, psychological quality, and lack of prospective assumptions and potential problems before surgery Bed traction combined with manual closed reduction of the fractured ends requires high surgical proficiency and surgical skills on the part of the operator and assistant. Strong basic knowledge and profound clinical practice experience are critical to the success of surgery. Physicians are kind and always maintain a humble attitude and the concept of being responsible to patients. An impetuous mood and surgical self-satisfaction strongly influence judgment. However, there is a lack of comprehensive surgical evaluation to predict potential problems and systematic postoperative protection. 5.6. There is a lack of confirmatory examinations after surgery Postoperative hip flexion and knee flexion check to determine the success of intramedullary pinning. This treatment lacks a sure-fire test, and there is no difference in length and varus deformity of the lower extremities. 5.7. Physical influence The patient was old, had long-standing history of rheumatoid arthritis, and had obvious osteoporosis. There is a possibility of postoperative screw loosening and screw removal due to shear tension, anatomical and biological stress, or improper limb function exercise and transfer. 5.8. Improper postoperative care and handling measures After the surgery, the affected limbs were guided by the doctor and the family members to follow the body's center of gravity in order to move in parallel, turn over, flex, and extend the limbs. When lying on the side, the center of the knee joints was suitable for materials and highly supported for the affected limbs, and the back was supported by the family members to stabilize the body balance. Violently turning over or carrying, improper movement of the affected limb or an unstable body center of gravity, sudden collapse of the body or natural sagging of the affected limb, placing the affected limb on top during lateral recumbency, and gravity or torsional stress may cause the screws to cut the cortical bone or nails. 5.9. Violation of doctor's orders Patients should rest in bed for one week after the surgery, after which they can do sit–stand training. When the patient has a concealed behavior, emotionally dominates the movement of the affected limb after returning home, or sits down for a long time, this could result in screw cutting and loosening. 5.10. Poor doctor–patient communication Poor doctor–patient communication involves a lack of good understanding between the doctor and the patient, misunderstanding in the exchanges between them, and poor implementation of the doctor's orders. There are many controversies between open reduction and closed reduction for subtrochanteric fractures of the femur. There is no significant difference between the two in terms of postoperative fracture healing, superficial tissue infection, and related complications (1, Temporary reduction and stabilization of fractures were performed with steel plates, and satisfactory results were obtained in the case of difficult reduction (15, Subtrochanteric fractures of the femur are unstable femoral fractures, which pose a risk of delayed union and non-union after treatment (32). There is currently no definitive treatment for implant rupture caused by delayed healing and non-union (33). Practitioners should generally follow moderate recommendations for the treatment of patients with unstable intertrochanteric fractures using a cephalomedullary device (34). Anti-osteoporosis treatment in elderly patients is also crucial. A patient with subtrochanteric fracture and implant rupture was treated with internal fixation with a long femoral nail. The implant was removed, and total hip arthroplasty was performed through a posterior approach, with satisfactory late results (35). In addition, the use of grooved tapered modular stems with distal fixation has potential advantages in femoral revision and post-traumatic situations (36). In terms of osteoporosis, patients were instructed to take calcium carbonate D3 for anti-osteoporosis treatment after surgery, without any other relevant intervention treatment. In conclusion, there is a possibility of surgical failure of the treatment of subtrochanteric Seinsheimer IIB fractures through various means, such as no anatomical reduction, deviation of the selected needle insertion point, selection of inappropriate surgical methods, mechanical and biomechanical effects, incompatibility of doctor–patient communication and cooperation, and non-doctor-ordered behaviors. According to the analysis of individuals, under the premise of an accurate needle entry point, minimally invasive closed reduction PFNA or open reduction of broken ends and intramedullary nail ligation for femoral reconstruction can be used in Seinsheimer type IIB fractures, which can effectively avoid the instability of reduction and the insufficiency of the biomechanics caused by osteoporosis. For clinical reference. The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author. The studies involving human participants were reviewed and approved by Ethics Committee of Feicheng Traditional Chinese Medicine Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. All the authors of this article participated in the whole process of the surgical treatment at the same time, as practitioners or assistants. The reasons for the failure of the operation were deeply analyzed, and conclusions and understandings were drawn. The first author collected, organized, and analyzed the data and edited and wrote the paper. All the authors jointly reviewed and revised the content of the paper. The authors do not have any conflicts of interest or disputes. All authors contributed to the article and approved the submitted version. This is a short text to acknowledge the contributions of specific colleagues, institutions, or agencies that aided the efforts of the authors. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. 1. Zhou ZB, Chen S, Gao YS, Sun YQ, Zhang CQ, Jiang Y. Subtrochanteric femur fracture treated by intramedullary fixation. CrossRef Full Text 2. Park SH, Kong GM, Ha BH, Park JH, Kim KH. Nonunion of subtrochanteric fractures: comminution or malreduction. CrossRef Full Text 3. Wang PC, Ren D, Song CH, Zhou B. Surgical technique for subtrochanteric fracture of femur. PubMed Abstract 4. Panteli M, Vun JSH, West RM, Howard AJ, Pountos I, Giannoudis PV. Management of subtrochanteric femur fractures: is open reduction associated with poor outcomes? PubMed Abstract 5. Joglekar SB, Lindvall EM, Martirosian A. Contemporary management of subtrochanteric fractures. PubMed Abstract 6. Delgado JM. Intramedullary nailing of subtrochanteric femur fractures in the lateral position. CrossRef Full Text 7. Freigang V, Gschrei F, Bhayana H, Schmitz P, Weber J, Kerschbaum M, et al. Risk factor analysis for delayed union after subtrochanteric femur fracture: quality of reduction and valgization are the key to success. PubMed Abstract 8. Zhong G, Teng L, Li H, Huang F, Xiang Z, Cen SQ. Surgical treatment of internal fixation failure of femoral peritrochanteric fracture. PubMed Abstract 9. Hsu KH, Chang CH, Su YP, Chang MC. Radiographic risk factors for predicting failure of geriatric intertrochanteric fracture treatment with a cephalomedullary nail. PubMed Abstract 10. Verettas DAJ, Ifantidis P, Chatzipapas CN, Drosos GI, Xarchas KC, Chloropoulou P, et al. Systematic effects of surgical treatment of hip fractures: gliding screw-plating vs intramedullary nailing. CrossRef Full Text 11. Rao DR, Krishna CSR. Study on functional outcome of subtrochanteric femur fractures treated with proximal femoral nail. CrossRef Full Text 12. Benz D, Tarrant SM, Balogh ZJ. Proximal femur fracture non-union with or without implant failure:a revision technique with clinical outcomes. PubMed Abstract 13. von Rüden C, Hungerer S, Augat P, Trapp O, Bühren V, Hierholzer C. Breakage of cephalomedullary nailing in operative treatment of trochanteric and subtrochanteric femoral fractures. CrossRef Full Text 14. Starr AJ, Hay MT, Reinert CM, Borer DS, Christensen KC. Cephalomedullary nails in the treatment of high-energy proximal femur fractures in young patients: a prospective, randomized comparison of trochanteric versus piriformis fossa entry portal. 15. Robertson R, Tucker M, Jones T. Provisional plating of subtrochanteric femur fractures before intramedullary nailing in the lateral decubitus position. PubMed Abstract 16. Zhao Z, Song F, Zhu J, He D, Deng J, Ji X, et al. Prone positioning for intramedullary nailing of subtrochanteric fractures, the techniques of intraoperative fluoroscopy and reduction: a technique note. CrossRef Full Text 17. Wang J, Li H, Jia H, Ma X. Intramedullary versus extramedullary fixation in the treatment of subtrochanteric femur fractures: a comprehensive systematic review and meta-analysis. PubMed Abstract 18. Kilinc BE, Oc Y, Kara A, Erturer RE. The effect of the cerclage wire in the treatment of subtrochanteric femur fracture with the long proximal femoral nail: a review of 52 cases. PubMed Abstract 19. Kulkarni SG, Babhulkar SS, Kulkarni SM, Kulkarni GS, Kulkarni MS, Patil R. Augmentation of intramedullary nailing in unstable intertrochanteric fractures using cerclage wire and lag screws: a comparative study. CrossRef Full Text 20. Gadegone WM, Shivashankar B, Lokhande V, Salphale Y. Augmentation of proximal femoral nail in unstable trochanteric fractures. PubMed Abstract 21. Codesido P, Mejía A, Riego J, Ojeda-Thies C. Subtrochanteric fractures in elderly people treated with intramedullary fixation: quality of life and complications following open reduction and cerclage wiring versus closed reduction. PubMed Abstract 22. Yoon YC, Oh CW, Oh JK. Biomechanical comparison of proximal interlocking screw constructs in different subtrochanteric fracture models. PubMed Abstract 23. Damany DS, Parker MJ, Gurusamy K, Upadhyay P. Complications of subtrochanteric fractures. A meta-analysis of 39 studies involving 1835 fractures. 24. Chockder AR, Anwaruzzaman S. Enhancement of stability of subtrochanteric fracture fixation by sign nail and plate augmentation. CrossRef Full Text 25. Knobe M, Drescher W, Heussen N, Sellei RM, Pape HC. Is helical blade nailing superior to locked minimally invasive plating in unstable pertrochanteric fractures? PubMed Abstract 26. Steensma M, Healey JH. Trends in the surgical treatment of pathologic proximal femur fractures among musculoskeletal tumor society members. PubMed Abstract 27. Persiani P, Noia G, de Cristo C, Graci J, Gurzì MD, Villani C. A study of 44 patients with subtrochanteric fractures treated using long nail and cerclage cables. PubMed Abstract 28. Förch S, Sandriesser S, Fenwick A, Mayr E. [Impairment of the blood supply by cerclages: myth or reality?: an overview of the experimental study situation]. CrossRef Full Text 29. Krappinger D, Wolf B, Dammerer D, Thaler M, Schwendinger P, Lindtner RA. Risk factors for nonunion after intramedullary nailing of subtrochanteric femoral fractures. PubMed Abstract 30. Chen B, Fan X. Pitfalls and remedial technique of intramedullary nail for subtrochanteric femur fractures: a case series. PubMed Abstract 31. Müller T, Topp T, Kühne CA, Gebhart G, Ruchholtz S, Zettl R. The benefit of wire cerclage stabilisation of the medial hinge in intramedullary nailing for the treatment of subtrochanteric femoral fractures:a biomechanical study. CrossRef Full Text 32. Teo BJX, Koh JSB, Goh SK, Png MA, Chua DTC, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. PubMed Abstract 33. O’Neill BJ, O’hEireamhoin S, Morrissey DI, Keogh P. Implant failure caused by non-union of bisphosphonate-associated subtrochanteric femur fracture. CrossRef Full Text 34. Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. CrossRef Full Text 35. Ozaki Y, Baba T, Ochi H, Homma Y, Watari T, Matsumoto M, et al. Total hip arthroplasty for implant rupture after surgery for atypical subtrochanteric femoral fracture. PubMed Abstract 36. Perticarini L, Rossi SMP, Fioruzzi A, Jannelli E, Mosconi M, Benazzo F. Modular tapered conical revision stem in hip revision surgery: mid- term results. PubMed Abstract
|